In the shadow of falling shells and the echo of distant gunfire, a different kind of battle is waged daily. It is not fought for territory or political ideology, but for the most fundamental human right: the right to health and life itself. In conflict zones across the globe, from the arid plains of sub-Saharan Africa to the besieged cities of the Middle East and Eastern Europe, healthcare represents the final, fraying thread of civilization. It is a fragile lifeline, perpetually at risk of being severed by violence, politics, and sheer neglect, yet held taut by the unwavering courage of medical personnel and humanitarian workers.
The concept of health in wartime transcends the mere treatment of bullet wounds and shrapnel injuries. It encompasses a vast and complex ecosystem of care that must adapt to a landscape of perpetual crisis. The immediate, visceral toll of conflict is evident in the trauma centers—makeshift facilities often located in basements, abandoned schools, or even tents. Here, surgeons perform life-saving amputations by the light of headlamps during power outages, and nurses ration dwindling supplies of anesthesia and antibiotics. Each patient represents a story interrupted by violence, and each successful treatment a small victory against the chaos. Yet, for every life saved on the operating table, countless others are lost to preventable causes, their access to care blocked by checkpoints, destroyed roads, or the simple, terrifying fact that a journey to a clinic could be a journey into a crossfire.
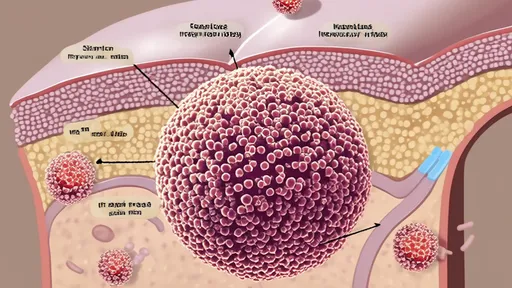
Beyond the visible trauma lies a deeper, more insidious health crisis. The destruction of critical infrastructure unleashes a cascade of public health disasters. Water treatment plants reduced to rubble force populations to rely on contaminated sources, sparking outbreaks of cholera and typhoid. The collapse of sanitation systems turns urban areas into breeding grounds for disease. Vaccination programs, the bedrock of preventative medicine, grind to a halt, allowing once-controlled illnesses like measles and polio to resurge with a vengeance. For those with chronic conditions such as diabetes, cancer, or heart disease, conflict is a death sentence. The supply chains for essential medicines are broken, and the specialized care they require becomes an impossible luxury. The mental health toll is perhaps the most profound and enduring scar. An entire generation is growing up knowing nothing but the sound of sirens and the sight of rubble, their psyches shaped by trauma, loss, and constant fear, with little to no access to psychological support.
In this harrowing environment, healthcare workers are more than just medical professionals; they are guardians of humanity. Their daily reality is one of impossible choices: deciding which patient gets the last unit of blood, navigating active sniper alleys to reach the wounded, and delivering babies in candlelit bunkers. They work under the constant threat of becoming targets themselves, in blatant violation of international humanitarian law. Hospitals, once sanctuaries, have too often been transformed into military objectives, their destruction not just a tactical maneuver but a catastrophic moral failure. The stress and burnout among these workers are immense, yet their commitment rarely wavers. They are the embodiment of the principle that medical care knows no borders, no sides, and no politics—only patients.
The international community's response to this crisis is a patchwork of heroism and heartbreaking insufficiency. Organizations like the International Committee of the Red Cross (ICRC), Médecins Sans Frontières (Doctors Without Borders), and the World Health Organization operate on the front lines, often at great personal risk. They negotiate humanitarian corridors that are too frequently violated, airlift supplies into contested areas, and train local staff to manage the overwhelming caseload. However, their efforts are perpetually hampered by a lack of safe access, chronic underfunding, and the politicization of aid. Aid convoys are blocked, and medical supplies are weaponized, held at borders as bargaining chips in a political game where civilian lives are the currency. This creates a situation where the very act of providing care becomes a political statement, further endangering both providers and recipients.
Ultimately, the struggle for health in conflict zones is a stark reflection of our collective conscience. It asks a fundamental question: in a world of unprecedented technological and medical advancement, why do we allow our most vulnerable to die from entirely preventable causes? The lifeline of health is not merely a medical necessity; it is a moral imperative. It is the foundation upon which any future peace must be built, for a population that is sick, traumatized, and without hope cannot rebuild a society. Ensuring the protection of healthcare is not an act of charity but a duty—a commitment to the idea that even in the darkest depths of war, the ember of our common humanity must be protected, for it is from this ember that the light of peace will one day be rekindled.

By /Oct 14, 2025

By /Oct 14, 2025

By Daniel Scott/Oct 14, 2025

By /Oct 14, 2025

By Benjamin Evans/Oct 14, 2025

By Ryan Martin/Oct 14, 2025
By John Smith/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025
By /Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By Amanda Phillips/Oct 14, 2025

By /Oct 14, 2025

By Megan Clark/Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025